Learn how to enable automatic payment allocations for Bulk Bill and DVA claims in Power Diary.
This article covers how to enable the system to automatically allocate a payment to invoices for paid Bulk Bill and DVA claims (AUS only), and discusses how this feature works. Once you've set this up, each time you run the Payment Report from the Medicare dashboard the system will automatically allocate a payment to each invoice that is returned as paid. If you haven't yet, please first read the articles on how to submit a Bulk Bill or DVA claim.
In this article:
How to turn on automatic payment allocations
By default, this setting will be switched off. When you go to Tools > Medicare you will see the status of the current settings, and this will reflect that the setting is disabled:
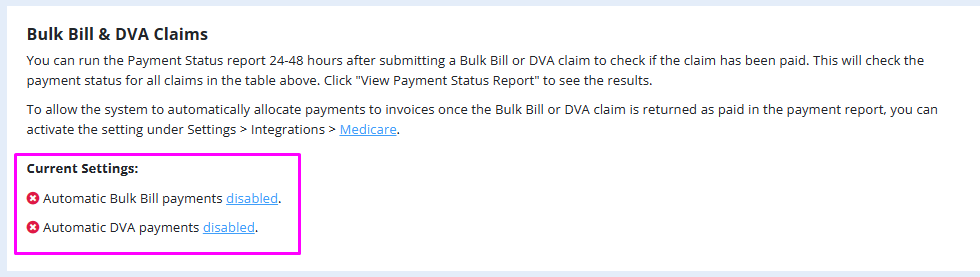
When the setting is disabled, when you click "Request Payment Status Report" and there are claims returned as paid, the system will not allocate any payments to the claim's invoices.
You can turn this feature on for either Bulk Bill claims or DVA claims, or for both. To enable the feature, follow these steps:
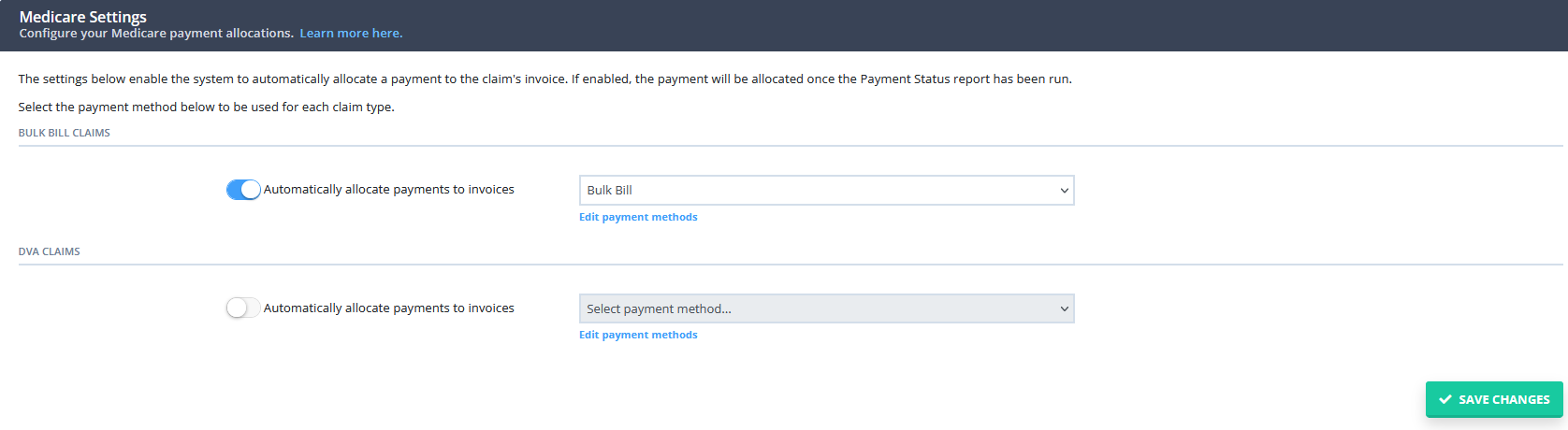
- Click on the 'disabled' link on the Current Settings.
- The system will take you to the Medicare settings page. On this page, switch on the slider for the claim type that you want to enable the feature for (either Bulk Bill or DVA)
- Select the payment method to be used for these payments
- Click "Save Changes"
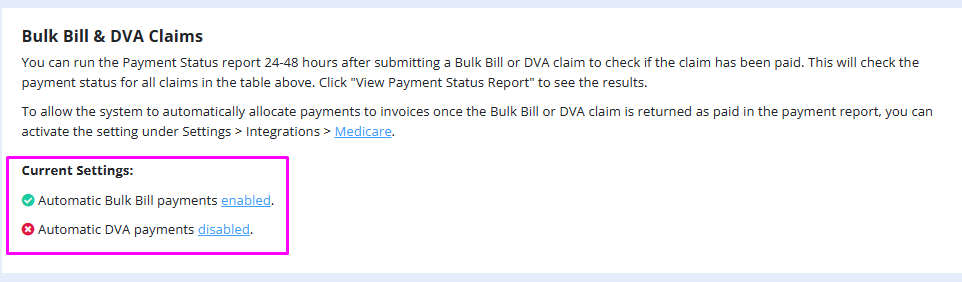
Once the setting has been enabled, you will see this reflected on the Medicare dashboard:
How the automatic payment allocations feature works
- Once the setting has been enabled, the system will then automatically create and allocate a payment to the invoice linked to the claim, once the claim been returned as paid in the payment report.
Read below for steps on how to fetch the payment report from the Medicare Dashboard for this to happen:
1. In Tools > Medicare > Filter the list of claims using the filters provided > Click "Search"Medicare processes Bulk Bill and DVA payments within 48 hours of claim submission. To ensure payments are processed, we recommend running the report at least 48 hours after submitting claims. Set the End Date filter to two days before the current date when running the report. If any claims remain unpaid, you’ll need to check their status manually later.2. Scroll down and click "Request Payment Status Report" (the report may take a few minutes to run depending on the volume of claims)
3. Any claims returned as paid in the report will have a payment automatically allocated to the invoice
4. Click "View Payment Status Report" to view the results
5. In the payment status report, view the "Payments Assigned" column - if this is checked this indicated a payment has been allocated by the system to the invoice
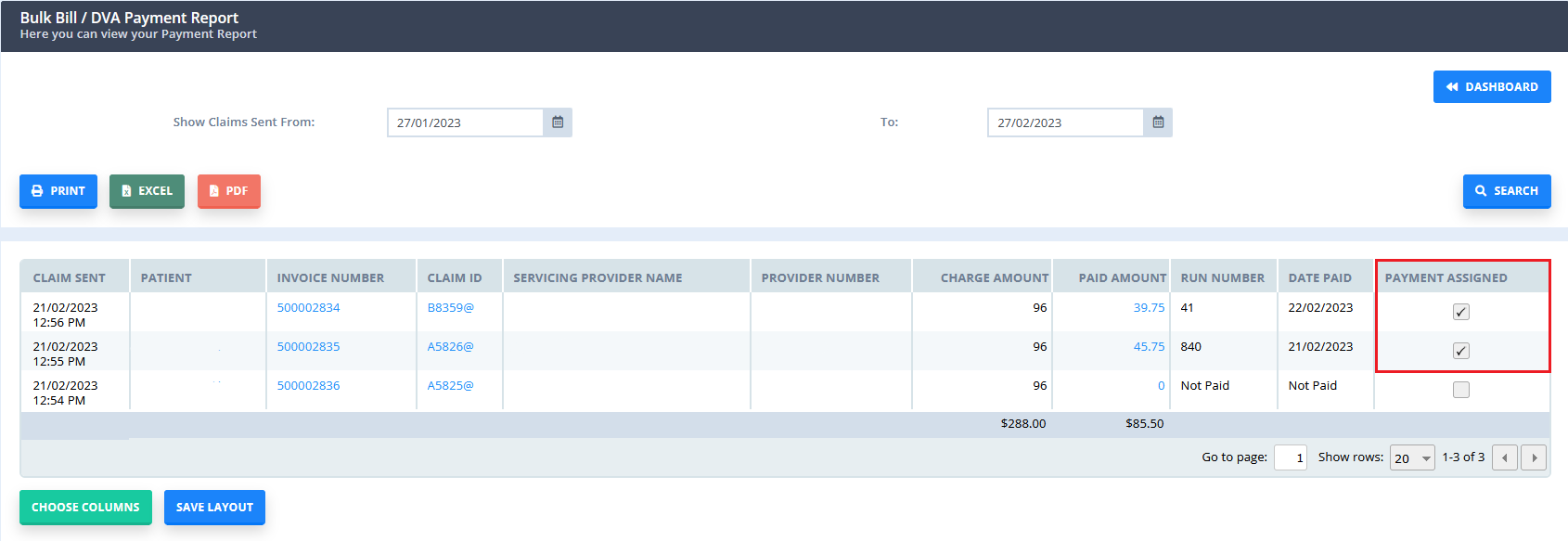
6. Right click on the invoice number to view the editing invoice page and view the payment.
7. If there are some past invoices that do not have the Medicare payments allocated, when you run the Request Payment Status Report, the system will allocate the payments, as long as the payment report is still available. Currently, Medicare payment reports are available during 6 months since the payment date.
Hint
The payment that is allocated to the invoice will be dated as received per the date that Medicare made the payment to you. The payment method used is based on the settings selected on the Medicare settings page (described above), and the payment note will show the payment run number. If the invoice is billed to a payee (such as a third party called "Medicare"), then the payment assigned will be from that payee, else it will be assigned to the client's
- Alternately, you can fetch the Payment Report for an individual claim:
- Access the claim
- Click the "Payment Report" button
- Click "Request Payment Report"
Important
Repeating the request for the payment report will not result in duplicate payments being allocated to the invoice. The system will only allocate one payment to the invoice. The payment can be deleted from the invoice, if you then re-request the payment status report the system will not allocate another payment.
