Learn how to set up Medicare Claiming on Power Diary, manage common errors, and ensure compliance.
Important
You must fill out your HW027 form to register for Online Claiming. If you or any providers that submit claims through your account have not filled out this form previously please do so immediately. Details on how to fill out the form and submit it to Medicare can be found here. Please keep Question 3 on the form blank.
When submitting Medicare claims you may run into errors that prevent the claim from being sent which are usually easily fixed if you know what to look for. We have put together a list of common errors below and explain how you might be able to fix each of them.
Once you have corrected the error you will need to resubmit the claim. You can do this in the same way that you submitted the claim originally.
Important
Please note that you cannot delete rejected Medicare claims. These will remain in the account.
In this article:
Claiming Errors and Response Codes
2017 : The Payee Provider specified is the same as the Servicing Provider
When the servicing provider is also the one receiving payment the payee provider fields need to be blank or Medicare will generate this error. To resolve this go to Settings → Practitioners → Practitioner name → Insurers (on the left). Edit the relevant Medicare insurer and remove the payee information. You can then resubmit the claim.
9201 : Invalid format for data item
This error simply indicates that some of the information provided is either incorrectly formatted or is missing. This is most commonly generated when the referring provider number is missing. To check this, simply scroll down and look over the data submitted and ensure that all required fields are filled and accurate.
9202 : Invalid Value For Data Item
There are few reasons why this error can occur:
- The patient has a PO Box as the address set up in the file
- The account holder of the patient has a PO Box attached to their file. A physical address is required, as a PO Box is not accepted by Medicare. This will need to be changed to a physical address
- If there is no date of birth entered or an invalid date of birth
- Service Type is selected incorrectly - see above for the instructions on how to fix this.
9202 : Invalid Value of [I] supplied for referral period code. The value supplied must be [S] (standard). Error located in medical event 1.
- This code/error refers to an (I) 'Indefinite' referral period entered under the Profile → Referrals which is not accepted for this particular claimant and/or claim. The Referral period should be set to (S) Standard (12 months from a GP and 3 months from a Specialist) or if Referral period set to Non standard, the period should be specified in the Service Text.
9501/9602 : This claim cannot be lodged through Medicare Easyclaim. Please submit the claim via an alternative Medicare claiming channel.
This error is commonly generated for a number of reasons:
- There is no referral listed or connected to the invoice being claimed when a referral is required for the item code being claimed.
- The client's details do not match medicare's database (i.e. client's full name, Medicare card number, or IRN). Please try validating the client's Medicare data in their profile and check if this returns a message that the data validates, or if there is a discrepancy with the data medicare has. If so, please confirm the correct details with the client.
- The client has met the maximum number of sessions possible under their referral (for example, all of the sessions within the mental health care plan).
9641 (or 9601) : Your claim was not able to be processed automatically due to a non-critical warning. You may try resubmitting the claim for manual processing.
This is a non-critical warning and as such can usually be ignored. To submit the claim and force it through simply click the green Resubmit Claim button or create a new claim and tick Accept Non Fatal Warnings toward the bottom right of the page prior to clicking Send. Once the claim has been submitted it will go through with a status of Pended.
9603 : Check the client's address. The address not entered is invalid.
When this error is appearing but the address appears to be correct (and the client has confirmed that the address matches what Medicare have on record) you may simply need to check that the spelling and format are correct. The easiest way to do this is to put the address into Google Maps and copy what they provide.
9630 : Please check the request or referral details.
This may mean that the referral details are incorrect, the referral has exceeded the number of appointments, or the referral date has expired. Because the Claim was immediately rejected, Medicare may have no record of this Claim. At that point, system checks may have found that the referral has exceeded the number of appointments which is why it stopped it from being submitted. It will require checking if the Provider Number of the Referring GP is correct, and/or checking with either the Referring GP or Medicare whether they've exceeded their number of appointments.
9632 : Duplicate of service already paid. If not duplicate resubmit with appropriate indication.
This type of error code comes up if there was more than one service performed for the client on the same day with the same item number and the same practitioner. You need to include additional information with the claim when you submit it to Medicare.
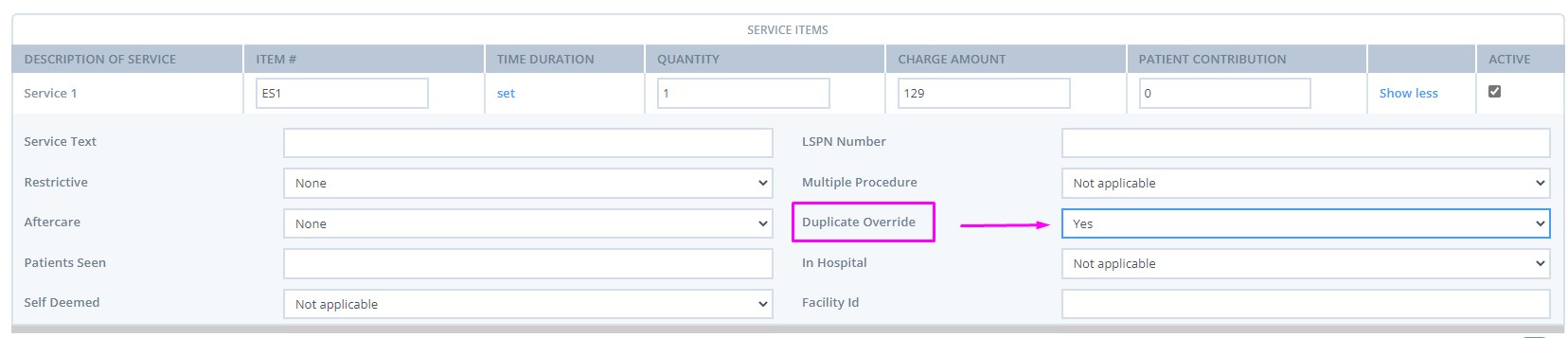
On the claim page, click on Show More on the Service Items section, and select Duplicate Override - Yes:
9650 : The card number and/or patient details submitted did not match Medicare checks. Please verify the details and resubmit with additional information if available.
The client's Medicare card number and/or address must be updated to match Medicare's files before the claim will be accepted.
2030: No referral is required for general service type claims
If the service type for the provider is set to "General Practitioner" the claim does not require a referral. If you are not a General Practitioner, change the service type to match the type of services provided.
If you navigate to Settings → Practitioners → Practitioner name > Insurers > Edit the Medicare insurance you will see the option to select the Service Type. in accordance with the services you provide.
9611: The item claimed is either unknown or invalid at the date of service. Eg Misc, incorrect alpha included.
Troubleshooting options:
1. Check Item code under MBS and ensure it matches format as well as correct code number.
2. Confirm with Medicare item number is correct for specific Service Item claimed.
3. Confirm with Medicare the Practitioner is able to claim the code or if Patient has to claim directly with Medicare.
Data Entry Notifications
Medicare Validation
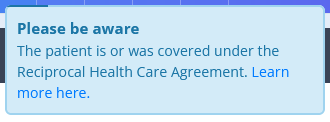
If a client is covered under Reciprocal Health Care Agreement and you validate their card, you will see this notification message. This is not an error, but just a notification for your information.
Invalid Medicare provider number: Alpha character does not match
This error is generated whenever the provider number that's entered doesn't exactly match what Medicare has on record. If the provider number is correct and this error is still being generated you can resolve it by placing a zero (0) at the start of the provider number and trying again.
The service type for the Provider is not consistent with the type of claim being submitted.
Please click “Edit Provider” (or go to Settings → Practitioners → Practitioner name → Insurers). Here, click the gear icon on the right to edit the insurance and select a service type that matches the type of claim being submitted:
- General Practitioner (Medicare / DVA Medical)
- Specialist & Allied Health (Medicare / DVA Medical)
- Pathology (DVA Medical)
- Community Nursing (DVA Allied Health)
- Speech Pathology (DVA Allied Health)
- Allied (DVA Allied Health)
- Psychology (DVA Allied Health)
The service type selected for the provider's insurance (Medicare or DVA) will need to be updated. The service type includes the type of claim that it can be used for in brackets after the service type name as shown in the list of service types below:
If you are submitting a Patient Claim or Bulk Bill, then you will need to choose a service type with the (Medicare / DVA Medical) label (i.e. General Practitioner or Specialist & Allied Health).
If you are submitting a DVA Medical/Paperless claim you will need to choose a service type with the (Medicare / DVA Medical) or (DVA Medical) label. (i.e. General Practitioner, Specialist & Allied Health, or Pathology)
If you are submitting a DVA Allied Health claim you will need to choose a service type with the (DVA Allied Health) label (i.e. Community Nursing, Speech Pathology, Allied, or Psychology).
If the client only has one name
In the event that the client only has one name, Medicare require that the name be entered in the surname / last name field. You can either replicate their name in both the first name and last name fields, or you can enter "Onlyname" in the first name field, and their name in the last name field. Both options will be accepted for claiming.
Important
- The list of all return codes for rejected Medicare claims can be found here.
- If the suggested solutions haven't worked for you please let us know so that we can assist you with the claim. In your email, please provide us with the invoice number relating to the claim so that we can investigate what might be causing the issue.
