Submit DVA claims easily with Power Diary. Follow our step-by-step guide for setup and submission. Ensure compliance and streamline your process today.
Important
You must fill out your HW027 form to register for Online Claiming. If you or any providers that submit claims through your account have not filled out this form previously please do so immediately. Details on how to fill out the form and submit it to Medicare can be found here. Please keep Question 3 on the form blank.
Once you have configured the DVA insurer, added your provider number(s) and recorded a client’s DVA details on their client record you are ready to begin submitting DVA claims through Power Diary. Follow on below to learn how!
In this article:
Submitting a claim
If you’re familiar with submitting Medicare claims through Power Diary then this process should feel very familiar. To submit a DVA claim follow the steps below.
Important
When submitting these claims you will need to ensure that you have the correct services configured (including the correct service code). You can learn more about how to set services up here.
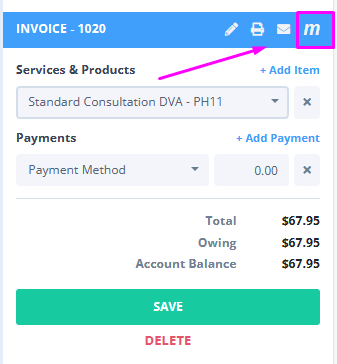
- On the appointment panel or edit invoice page, select the Medicare button.
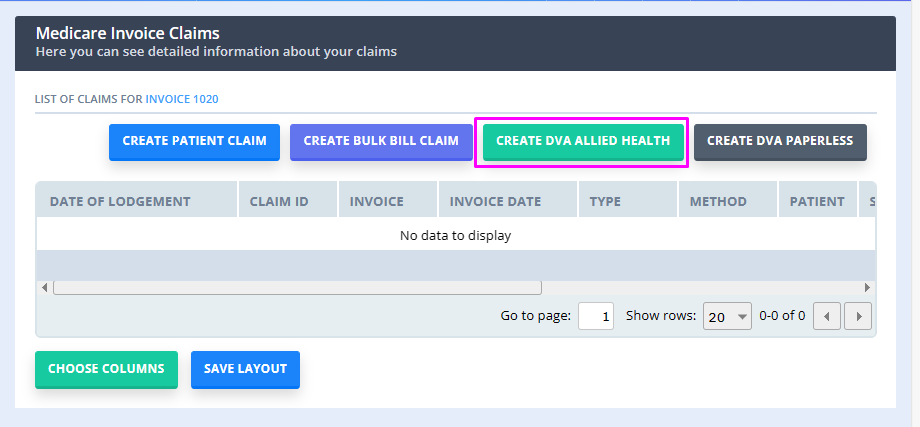
- Select either Create DVA Allied Health (for allied health, community nursing, psych, and speech pathology) or Create DVA Paperless (for specialists and GPs) depending on which type of claim you would like to submit.
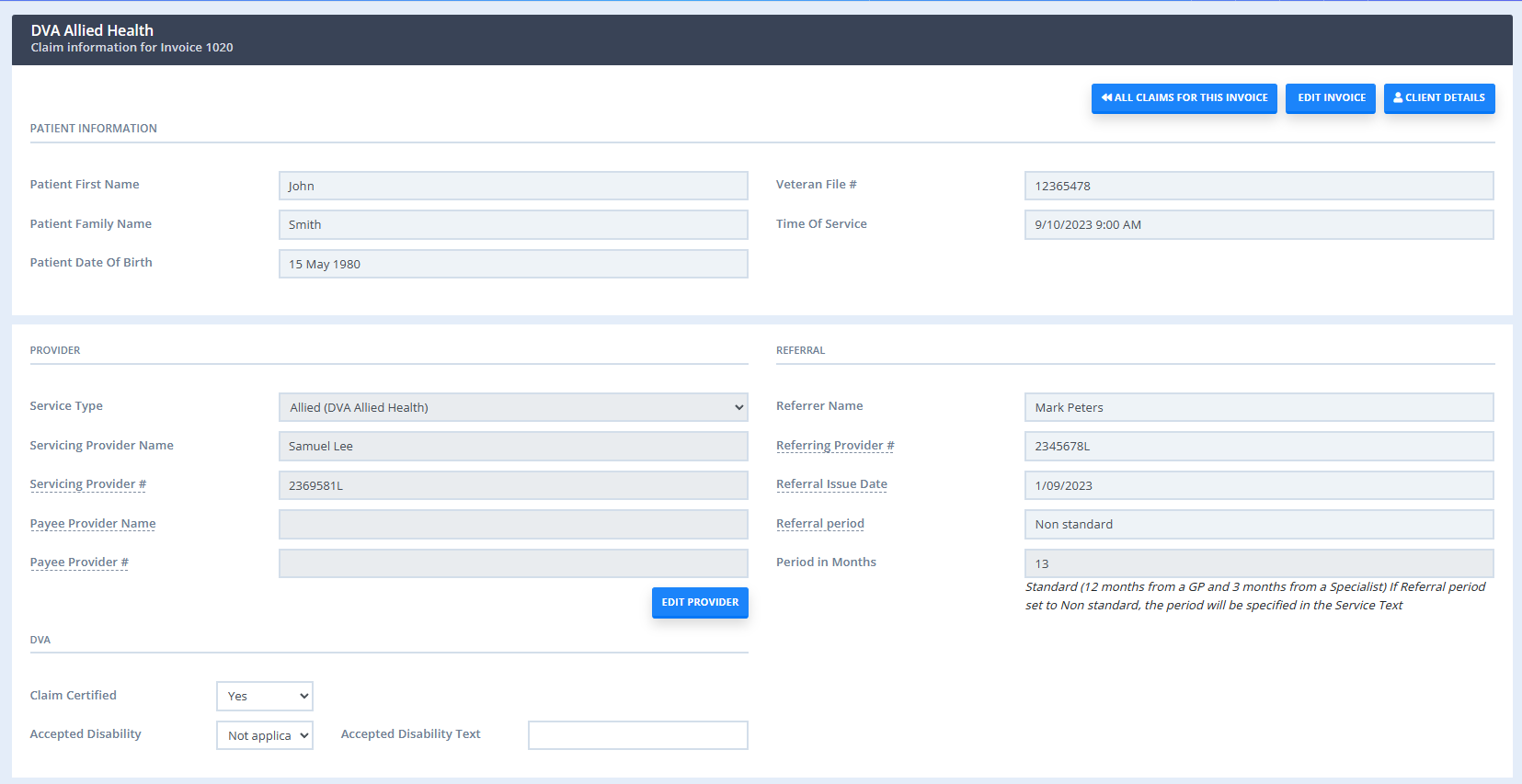
- Most of the information will be automatically filled out for you, such as patient and provider information and referral information (if this was selected on the invoice). You will only need to input a small amount of information such as the treatment location.
- Once you have filled out any relevant information simply click Send or Save and Send Later (if you would like to submit multiple claims at once at a later time).
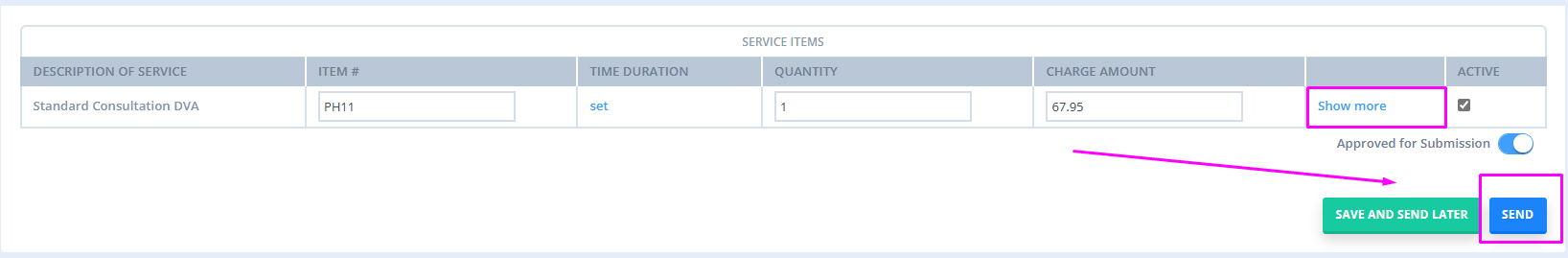
And that’s it! Your claim should go through with a status of Referred if it was successful. If you receive another message you should be able to follow the prompt to troubleshoot and resubmit.
For information on cancelling a DVA claim, please refer to our article here: DVA claims: Troubleshooting and Frequently Asked Questions.
Understanding the DVA fields
When submitting DVA claims you will need to fill out a few fields (accessible via Show More field) that you may be unfamiliar with (especially if you are used to claiming through a service such as PRODA). The tables below should help in filling this section out.
Treatment Location
Only applicable for DVA Medical Paperless claims. In the majority of situations, R will be selected, indicating rooms (such as your practice).
| Values | Constraints | Conditions |
|---|---|---|
|
None H = Hospital R = Rooms |
Only required for General or Specialist service types. If the referral override code is set to H then the treatment location code must |
This code specifies where the treatment or service was provided. |
Claim Certified
| Values | Constraints | Conditions |
|---|---|---|
| Y = The provider acknowledges certification obligations. | This will default to 'Y' if the Claim Certified Date is set. | Indicates that the provider has certified the services within the claim have been provided. Must be set to 'Y' to submit the claim. |
| N = The provider does not acknowledge the certification (Not valid for DVA Allied Health and Community Nursing). | - | - |
Accepted Disability
Set this to Y if the patient is a DVA White Card holder. If you set this to Y then you also have to fill out the Accepted Disability text field below which is used to describe the condition that was treated during the session being claimed.
| Values | Constraints | Conditions |
|---|---|---|
| Y = Condition treated relates to a White Card holder | If set to 'Y' the Accepted Disability test must be present otherwise value must be 'N'. | Indicates whether the services rendered are for a White Card holder and the service is in accordance with the White Card condition. |
| Not Applicable = Condition does not relate to a White Card holder | - | - |
Accepted Disability Text
| Values | Constraints | Conditions |
|---|---|---|
| 1-100 Characters Alphabetical characters [A-Z], numbers (0-9), spaces, and the following special characters : ; , . - The first character must be alpha or numerical. No spaces can appear before or after the text. |
Must be set when the Accepted Disability is set to 'Y'. |
Free text used to provide details regarding the condition being treated. |
Understanding the Service Item fields
When viewing the table of service items, if you click "Show More" you will see several additional fields that can be filled in. This section explains what these fields are used for and when they should be filled. For more information on these fields please see Medicare's website here.
Service Text
Free text used to provide additional information to assist with the assessment of the service.
| Values | Constraints | Conditions |
|---|---|---|
| 1-100 Characters Special characters permitted: @ # $ % + = : ; , . - |
Must be set when Multiple procedures Override is set to 'Y'. Must be set when Restrictive Override Code is set. Must be set when Duplicate Override Code is set. |
Use service text to provide the reason for the override. |
Account Reference Number
Optional field to record a reference to identify the claim (such as invoice number)
| Values | Constraints | Conditions |
|---|---|---|
|
Alpha (A-Z) or Numeric (1-9) |
- | - |
Restrictive (override code)
This code is used to allow payment for services where the account provides indication that the service is not restrictive with another service within the same claim or on the patient history.
| Values | Constraints | Conditions |
|---|---|---|
| Separate Sites Not Related (Care Plans for allied health) Not for Comparison |
- | If set, service text must be set to provide the reason for the override. |
Aftercare
Only applicable for DVA Medical Paperless claims. Indicates whether or not the service was performed as part of normal aftercare for the patent (post-operative care and treatment including all attendances until recovery).
| Values | Constraints | Conditions |
|---|---|---|
| For aftercare. Not for aftercare. |
- |
Patients Seen
Only applicable for DVA Medical Paperless claims. List the number of patients seen for the service.
| Values | Constraints | Conditions |
|---|---|---|
| 1-99 | Must be set for group attendance or visits (to home, hospital, or institution) to ensure the correct payment is made. | List the number of patients seen for the service. |
Self Deemed
These services do not require a referral.
| Values | Constraints | Conditions |
|---|---|---|
| SD = Self Deemed SS = Substituted Service |
Must not be set for General Practitioner service types. Must not be set to SS for Pathology service types. Must not be set when Referral Override Code is set. |
A Self Deemed service is a service provided by a consultant physician or specialist as an additional service to a valid request. A substituted service is a service provided that has replaced the original service requested. |
Distance Kms
Indicates travelling distances involved in a home, nursing home, or hospital visit.
| Values | Constraints | Conditions |
|---|---|---|
| 11-999 | Must not be set for Community Nursing service type. Must be a minimum of 11. |
Claim distance travelled for out-of-room visits. The first 10km is not payable. |
Second Device
Only applicable for DVA Allied Health claims. This field identifies the provision of second medical grade footwear service.
| Values | Constraints | Conditions |
|---|---|---|
|
Y = Yes. |
This field is only relevant to podiatrists. Must only be set for Allied service type codes. |
This field identifies the provision of second medical grade footwear service. |
LSPN Number
Only applicable for DVA Medical Paperless claims. Location Specific Practice Number used for diagnostic and radiation oncology that is specific to an individual location.
| Values | Constraints | Conditions |
|---|---|---|
| Numeric ≥ 1 | Must not be set for Pathology service types. Must not be set with number of Patients Seen. Must not be set with Time Duration. |
Only one LSPN Number can be set per claim. |
Multiple Procedures (override)
Only applicable to DVA Medical Paperless claims. Indicates whether the multiple services rule should or shouldn't be applied to the services being claimed.
| Values | Constraints | Conditions |
|---|---|---|
| Yes = Not multiple No = Multiple |
Must not be set for Pathology service type. |
Used for claiming multiple item codes at once that are not duplicate services. If set to Yes (i.e. the items are not duplicate services), Service Text must be set to provide the reason for the override. |
Duplicate (Services) Override
Indicates whether multiple services performed on the same day, by the same service provider should be treated as separate services.
| Values | Constraints | Conditions |
|---|---|---|
| Yes = Not duplicate No = Duplicate |
Must not be set for Pathology service type. |
Used for claiming multiple item codes for the dame day that are not duplicate services. If set to Yes, Medicare Event Time or Service Text must be set to provide the reason for the override. |
In Hospital
| Values | Constraints | Conditions |
|---|---|---|
| Yes = In Hospital No = Not in hospital |
- | The value must be set to Yes if the service was provided in the hospital. |
Facility Id
The Commonwealth Hospital Facility Provider Number. A unique identifier of a Registered Hospital or Day Care Facility.
| Values | Constraints | Conditions |
|---|---|---|
| 8-digit provider number. | - | Can be set for in-patient hospital claims. |
Specimen Collection Point
Only applicable to DVA Medical Paperless claims. Used to identify the site where the pathology specimen was collected.
| Values | Constraints | Conditions |
|---|---|---|
| 3-4 characters long Alpha (A-Z) or numeric (0-9). | - | If set, either the referral override code must be set to N, or the Self-Deemed code must be set to SD. |
Admission date
Only applicable for DVA Allied Health claims. The date the patient was admitted to hospital.
| Values | Constraints | Conditions |
|---|---|---|
| Date | Must be set for Community Nursing service type only. Must not be set after the medical event date (i.e. appointment date being claimed). |
For DVA Community Nursing, this is the admission date to the nursing service. |
Discharge Date
Only applicable for DVA Allied Health claims. The date the patient was discharged from hospital.
| Values | Constraints | Conditions |
|---|---|---|
| Date | Must be set for Community Nursing service type only. Must not be set before the admission date. Must not be a future date. |
Date of discharge from hospital. |
